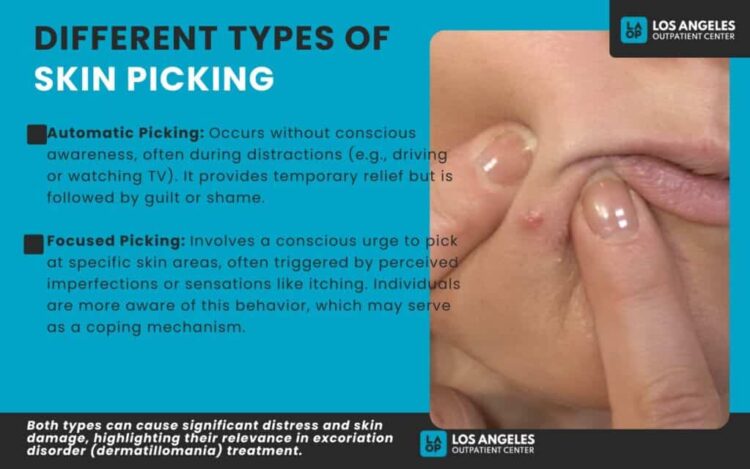
Skin picking, also known as dermatillomania or excoriation disorder, is a compulsive behavior that can cause physical harm and emotional distress. Therapy plays a critical role in managing this condition by addressing the underlying triggers and teaching coping strategies. Effective therapy for skin picking helps reduce the urge to pick and improves overall well-being through targeted behavioral techniques and emotional support.
Many individuals find success with cognitive-behavioral therapy (CBT), which helps them recognize patterns and replace harmful actions with healthier habits. Therapy can also include other approaches such as habit reversal training or creative therapies that provide alternative outlets for emotions and stress.
Understanding the connection between skin picking and mental health is essential for lasting change. With professional guidance, individuals can regain control over their behavior and significantly reduce the impact of skin picking on their lives.
Therapy for Skin Picking: Types and Effectiveness
Therapeutic approaches for skin picking focus on reducing urges, managing symptoms, and preventing tissue damage. Several well-studied methods include behavioral techniques and cognitive strategies tailored to individual needs and symptom severity.
Cognitive Behavioral Therapy Approaches
Cognitive Behavioral Therapy (CBT) targets the thoughts and behaviors that trigger skin picking. It helps patients identify and challenge distorted beliefs related to their urges. The therapy focuses on increasing awareness of triggers and developing coping strategies to manage compulsions.
CBT has demonstrated effectiveness in decreasing the frequency and intensity of skin picking. Techniques often include exposure and response prevention, where individuals practice resisting picking in controlled situations. This reduces anxiety and compulsion over time.
Therapists may also use cognitive restructuring to replace negative thoughts with realistic, supportive ones. Combining these elements makes CBT a widely recommended treatment for skin picking disorder.
Habit Reversal Training Strategies
Habit Reversal Training (HRT) is a behavioral intervention that replaces skin picking with healthier habits. It involves awareness training to recognize early signs of picking and competing response training to engage in alternative behaviors instead.
For example, when a picking urge arises, patients learn to clench their fists or hold a stress ball. This physical substitution interrupts the automatic picking behavior. HRT also teaches relaxation techniques to reduce underlying anxiety or tension.
Clinical studies show HRT reduces symptom severity and improves control over skin picking urges. It provides practical, skills-based tools that patients can apply in daily life, increasing independence in managing the disorder.
Mindfulness-Based Techniques
Mindfulness strategies cultivate non-judgmental awareness of thoughts and bodily sensations linked to skin picking. Patients practice observing urges without reacting, creating distance between impulse and action.
These techniques include focused breathing, body scans, and mindful meditation. Mindfulness helps reduce emotional reactivity, which often fuels picking episodes. It promotes acceptance rather than avoidance of uncomfortable sensations.
Evidence suggests mindfulness reduces compulsive behaviors and associated distress. It may be especially useful when combined with other therapies to enhance overall emotional regulation.
Acceptance and Commitment Therapy for Skin Picking
Acceptance and Commitment Therapy (ACT) encourages patients to accept their urges without trying to control or eliminate them directly. Instead, it focuses on committing to value-driven actions that improve quality of life despite symptoms.
ACT teaches psychological flexibility by helping individuals observe urges, accept emotional discomfort, and redirect attention to meaningful activities. This reduces the power of urges to dictate behavior.
In skin picking disorder, ACT has shown promise in decreasing symptom severity and distress. It is often incorporated with behavioral strategies to address both acceptance and behavior change simultaneously.
How to Begin Treatment and Support Recovery
Starting treatment for skin picking involves locating professional help, using practical self-help strategies, and engaging close support systems. Each of these elements plays a critical role in establishing a foundation for recovery and ongoing management.
Finding a Qualified Therapist
Identifying a therapist with experience in treating excoriation disorder is essential. Cognitive-behavioral therapy (CBT), specifically habit reversal training, is the most evidence-based approach.
Look for clinicians specializing in body-focused repetitive behaviors or obsessive-compulsive related disorders. Many therapists now offer online sessions, which increases access for people unable to attend in person.
Verification of credentials and treatment focus can be done through professional directories or mental health organizations. It is important the therapist creates a structured plan with clear goals, addressing both compulsive behavior and any emotional triggers.
Self-Help Tools and Resources
Practical self-help techniques work alongside therapy to reduce skin picking episodes. Using physical barriers like hydrocolloid patches or bandages helps prevent direct contact with the skin. These also promote healing of affected areas.
Habit tracking, mindfulness exercises, and stress reduction strategies support emotional regulation. Structured plans that define risky behaviors and recovery actions make daily progress measurable.
Resources such as workbooks, support groups, and online communities provide tools and motivation. Combining these approaches helps maintain long-term progress outside therapy sessions.
Involving Family or Support Networks
Supportive family members or friends can help monitor and manage skin picking behaviors. Educating them about excoriation disorder encourages understanding and reduces stigmatization.
They can assist by gently reminding the person to use coping tools in moments of difficulty or redirect attention from picking urges. Participation in therapy sessions or support groups, when appropriate, strengthens the recovery environment.
Clear communication about boundaries and needs is necessary to avoid frustration on all sides. A reliable support network offers accountability and emotional encouragement vital for sustained recovery.