Introduction
Your time in physical therapy should be spent making patients whole again and getting them stronger — not pursuing payments. But let’s be real: a single billing error can hold up reimbursement or trigger claim denials that drain your clinic’s revenue.
Physical therapy billing isn’t paperwork; it’s the backbone of your financial well-being. Properly done, it guarantees steady cash flow and insurance rule compliance. Improperly done, it causes undue stress and brings your business to a halt.
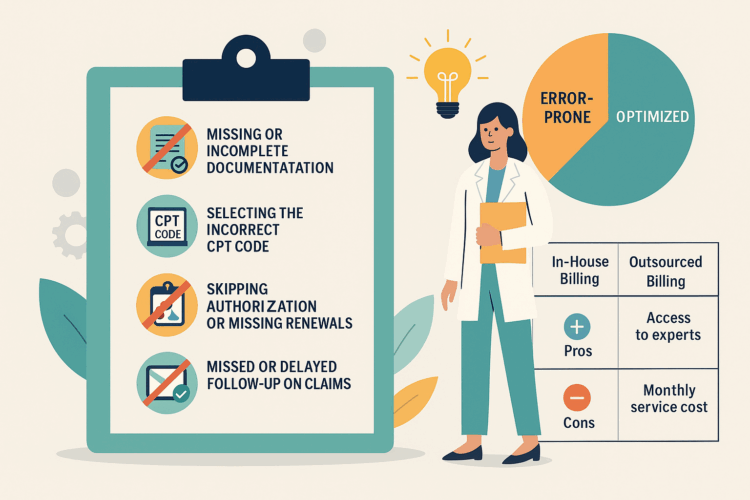
Let’s examine each of the top five billing errors physical therapy clinics experience — and how to avoid them so you can focus on what matters most: your patients.
1. Missing or Incomplete Documentation
Poor or incomplete documentation is one of the leading causes of claim denials.
Most physical therapy clinics underappreciate how thorough their documentation must be. Payers for insurance demand each treatment, test, and follow-up to be substantiated by full clinical documentation.
If your documentation fails to align with the billed CPT code, your claim will get rejected or flagged.
For instance, if you bill for a moderate complexity evaluation but document it like a low-complexity case, that’s a red flag.
How to avoid the error
- Take clear, detailed notes at the conclusion of every session.
- Ensure that your documentation corresponds to the billed treatment level.
- Maintain updated standardized templates for all the providers within your clinic.
If you require a reminder about correct code usage, have a look at this PT Guide — it describes how to correctly use and bill CPT code 97162 and may assist you in getting your physical therapy billing documentation aligned with payer requirements
2. Selecting the Incorrect CPT Code
Physical therapy billing codes get confusing when several evaluation codes seem to be the same. Codes 97161, 97162, and 97163 all reflect varying levels of complexity — and getting it wrong can impact your payments.
For example, charging 97163 (high complexity) for a moderate case may appear to be overcharging, and charging 97161 (low complexity) on a detailed evaluation is undercharging for your time.
This is how to do it correctly:
- Understand the criteria for each CPT code.
- Match the code to your documentation — not your assumption.
- Review payer-specific coding rules every few months.
Getting the codes right means you’re not leaving money on the table or exposing your clinic to compliance risks.
3. Skipping Authorization or Missing Renewals
Skipping over prior authorization is probably the simplest way to lose money. A few clinics count on an authorization already on file to cover every session — but after it expires, extra visits become billables.
Insurers are tough on these timelines, and one missed renewal deadline can trigger multiple claim denials.
Prevention tips:
Always check insurance coverage before every visit.
- Track authorization start and end dates in an easy-to-use dashboard or spreadsheet.
- Designate one employee to manage renewals and verification follow-ups.
- It takes only a little effort up front to save hours of rework and appeals in the future.
4. Missed or Delayed Follow-Up on Claims
You’ve submitted your claim — but that’s not the end of the story. Many clinics lose thousands each year because they never follow up on denied or pending claims. It’s a quiet revenue leak that builds up over time.
Claims need active tracking. The longer a denial sits untouched, the harder it becomes to recover payment.
Here’s a simple look at how follow-up timing impacts claim recovery:
The takeaway: Prompt follow-ups are a big help.
What you can do:
- Check unpaid claims on a weekly basis.
- Sort them by denial cause (coding error, missing docs, payer delay).
- Resubmit reworked claims straight away.
A structured AR (Accounts Receivable) function can convert missing claims into recovered revenue.
5. Neglecting Industry News and Compliance Updates
Insurance policies, CPT codes, and billing guidelines get updated regularly. Not keeping yourself current exposes your clinic to compliance violations or under-payments.
For instance, a small change in documentation practices or coding guidelines can result in a claim otherwise in perfect order being rejected.
Get ahead by:
- Participating in billing webinars or brief trainings every three months.
- Signing up for professional newsletters which monitor CPT updates.
- Utilizing billing software that emphasizes recent changes.
If professional assistance is your desire, think of services such as aba therapy billing. Although it’s mostly designed for behavioral health and therapy practitioners, their systematic way of handling claim accuracy, denial management, and compliance can be an excellent model for physical therapy clinics as well.
How Proper Billing Practices Help Your Clinic Grow
When your billing is timely and accurate, everything else at your clinic flows more smoothly. Staff are paid on time, patients have fewer billing issues, and less time is spent correcting errors.
Here’s a quick chart illustrating the difference between error-prone billing and optimized billing:
| Category | Error-Prone Billing | Optimized Billing |
| Claim Denials | 15%–25% | Below 5% |
| Average AR Days | 45–60 | 18–25 |
| Staff Productivity | Low | High |
| Revenue Growth | Slow or Flat | Steady Increase |
It’s not a matter of working harder — it’s a matter of working smarter and implementing a system that promotes accuracy and consistency.
Pros and Cons of Doing Billing In-House Versus Outsourcing
| Method | Pros | Cons |
| In-House Billing | Full control, immediate communication with staff. | Time-consuming, higher training costs, prone to internal errors. |
| Outsourced Billing | Access to experts, fewer denials, faster collections. | Monthly service cost, requires trust in the partner. |
It all depends on the size and capacity of your clinic. Most small-to-medium-sized practices find outsourcing to be more efficient as it minimizes administrative strain and promotes compliance.
Conclusion
Physical therapy billing mistakes aren’t just frustrating — they’re costly. One missed detail can delay hundreds or thousands of dollars in payments. The good news is that with the proper awareness and easy process enhancements, most billing issues are entirely preventable.
By documenting accurately, coding correctly, tracking authorizations, following up on claims, and staying updated on changes, your clinic can maintain a healthy cash flow and stronger patient focus.
To sharpen your understanding of correct code usage, revisit the PT Guide. And if you’re exploring reliable billing support, look into aba therapy billing — their streamlined approach helps therapy practices reduce denials and boost collections efficiently.
Correct billing isn’t only about being paid. It’s about providing your practice with the financial stability it requires to continue providing excellent care — each and every day.